Urinary tract infections (UTI): a burning topic
Urinary tract infections (UTI) – also sometimes referred to as ‘cystitis’ or ‘bladder infection’ – are bacterial infections in the urinary system. The urinary system includes the bladder, kidneys, ureters (tubes that go from the kidneys to the bladder) and urethra. UTIs are quite common and usually not serious, but if you’ve ever experienced one, you know how serious they can feel and how urgently you need treatment to address the issue.
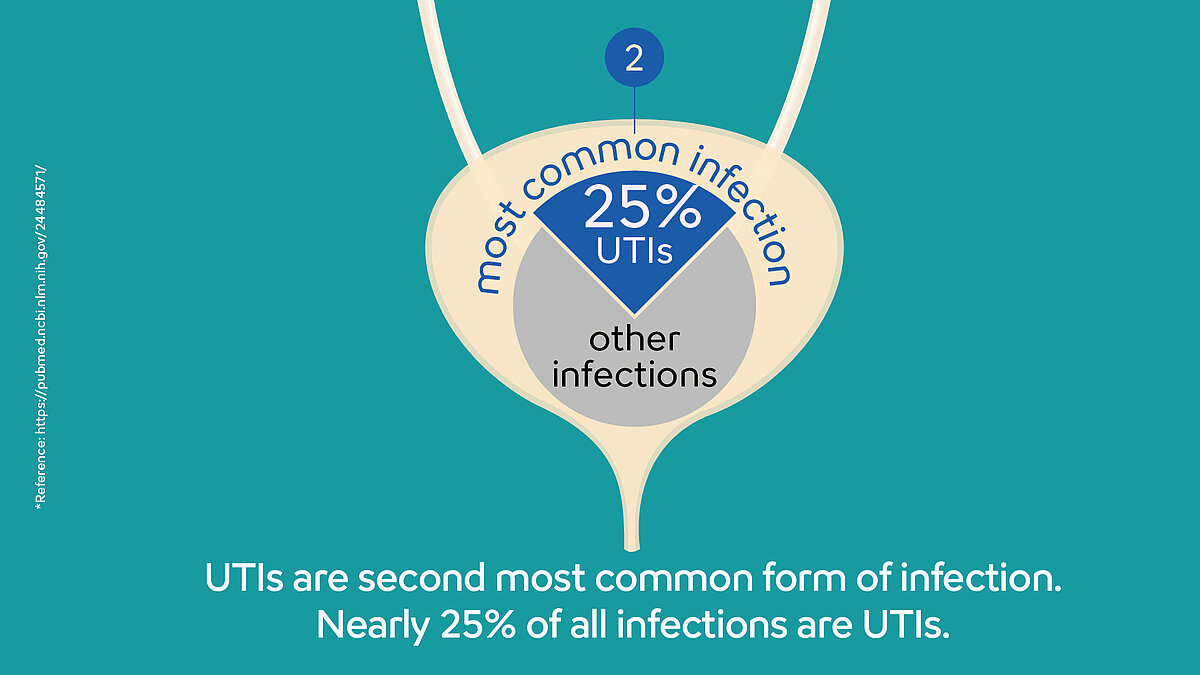
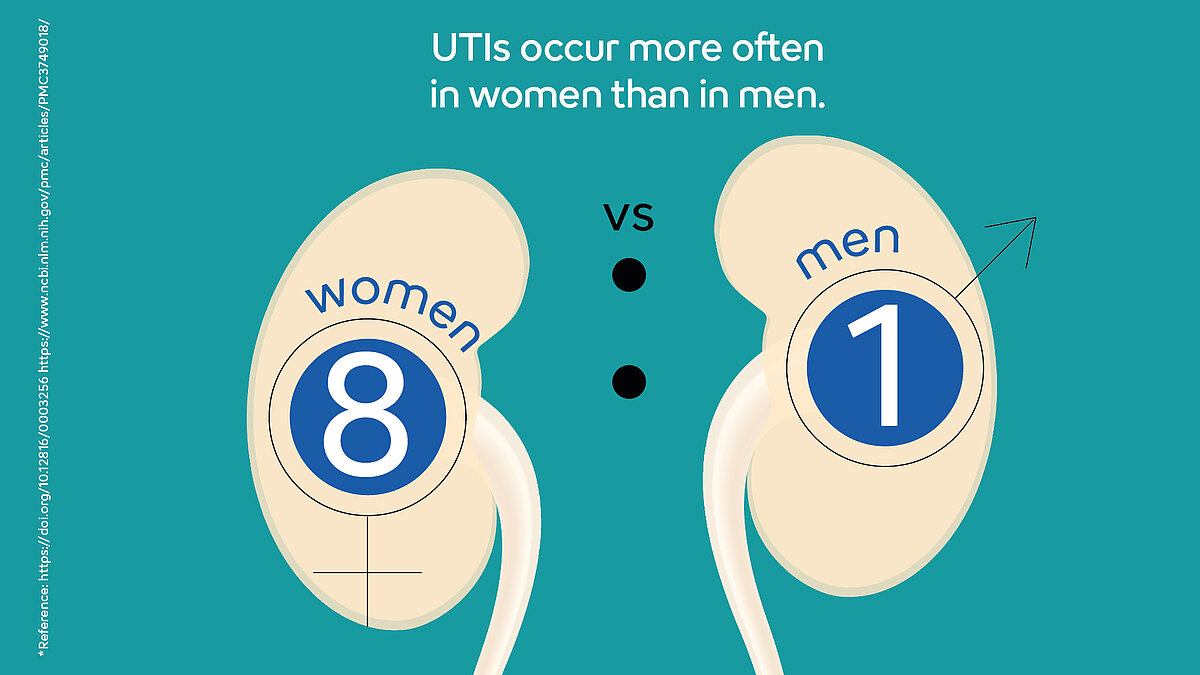
Most UTIs are due to bacteria that are normally found in your digestive tract, such as E. coli., although other bacteria can cause them as well. Many types of bacteria live in the intestines, but because urine is sterile, the urinary system is typically bacteria-free. So when rogue bacteria are introduced into the urinary system, it can trigger a UTI. In most cases, bacteria travel up the urethra to the bladder. It is estimated that 150 million UTIs occur yearly on a global basis, making it one of the most frequent bacterial infections worldwide. Of those affected by a UTI, only about 0.05% are estimated to be men.
It seems that UTIs tend to favour women based on their anatomy. Nearly one in three women will have had a UTI requiring antibiotic treatment by the age of 24. Women are more likely to get urinary tract infections because the urethra is much shorter than in men. Because the urethral opening is closer to the anus in women, it’s easier for bacteria from stool to also find its way into the urethra. In men, a UTI is almost always a symptom of another condition. Oftentimes, the infection has moved from the prostate or some other part of the body, or it may mean that something is blocking the urinary tract.
Fill up the cup – the lab does the rest
The first step in diagnosing a UTI is typically a simple urinalysis test, done using a urine sample. It looks for signs of bacteria as well as abnormal counts of white and red blood cells. Most often this is done by using a dipstick test, or a urine test strip. It is quick, but not the most accurate or reliable method because it can result in a false negative.
A more precise alternative is urine culture testing in a laboratory; therefore, when suspecting a UTI, your physician might also decide to send your urine sample there to be tested. The laboratory confirms the bacterial infection and performs antibiotic susceptibility testing (AST) to assess the effectiveness of individual antibiotics in killing the bacteria causing the infectious episode. This is the ideal scenario in terms of specificity because guessing and getting the wrong antibiotic can lead to an increase in antibiotic resistance among urinary tract pathogens. Lab testing takes a bit longer, however, typically requiring 2-3 days until results are available.
Antibiotic susceptibility testing in a near-patient setting bridges the gap between urine test strips and the time required for a lab analysis. New technologies make it possible to test a range of the most common antibiotic treatments for uncomplicated UTIs in a very short time and in close proximity to the patient– without first sending samples to the lab. Bacteria from urine samples are isolated and investigated by exposing them to a selection of antibiotics and monitoring their reaction in real time. Actionable results are produced quickly, helping physicians make a fast treatment decision, and thereby avoiding unnecessary treatments that lead to an increase in antimicrobial resistance. As a supplemental diagnostic tool, AST in near-patient settings does not fully replace lab testing for less common antibiotics or more difficult cases; instead, it adds a new capability to support expedited and improved treatment at the point of care.

What happens after being diagnosed with a UTI?
There are both holistic and medical treatments, or a combination of both, that are recommended by healthcare professionals. Drinking lots of fluids is sometimes suggested in order to flush out the bacteria by emptying the bladder more frequently. You may have also heard or seen on some medical websites that drinking cranberry juice can help prevent UTIs and/or help get rid of them. Some studies suggest it can help prevent an infection because cranberries contain a substance that prevents E. coli bacteria from sticking to the walls of the bladder. Without sticking to the wall, bacteria such as E. coli can’t infect the urinary tract. You can find countless anecdotes from online commenters swearing that it works for them, despite the contradictory scientific evidence. While the effectiveness of cranberry juice and other more holistic treatments is disputed, correctly administered antibiotics certainly are effective, making them the first-line treatment for UTIs.
Prescription antibiotics will almost always cure a UTI; therefore, treatment is usually straightforward. However, in recent years, this has become more complicated due to the over-prescription of broad-spectrum antibiotics. It’s important to consult a physician if you think you may have a UTI so you can get the proper antibiotic treatment.

Still want to know more?
Visit our AMR (antimicrobial resistance) page to learn even more about how it’s crucial to use antibiotics and other antimicrobial treatments in the right way.
References
[1] Blahd, W. MD (reviewed by). (2017): Slideshow: A Visual Guide to Urinary Tract Infections
[2] Bandukwala, N.Q. DO (reviewed by). (2018): What Are Urinary Tract Infections (UTIs)?
[3] Cox, D. (2017): Everything you ever wanted to know about urinary tract infections.
[4] Jepson, R. G., Williams, G., & Craig, J. C. (2012): Cranberries for preventing urinary tract infections. The Cochrane Library
[5] Krieger, J. N., Ross, S. O., & Simonsen, J. M. (1993): Urinary tract infections in healthy university men The Journal of urology, 149(5), 1046-1048.
[6] Pevzner, H. (2018): How to Prevent Urinary Tract Infections or UTIs
[7] Raz, R., Chazan, B., & Dan, M. (2004): Cranberry juice and urinary tract infection. Clinical infectious diseases, 38(10), 1413-1419.
[8] Jenny Stamos Kovacs (2021): Urinary Tract Infections (UTIs)