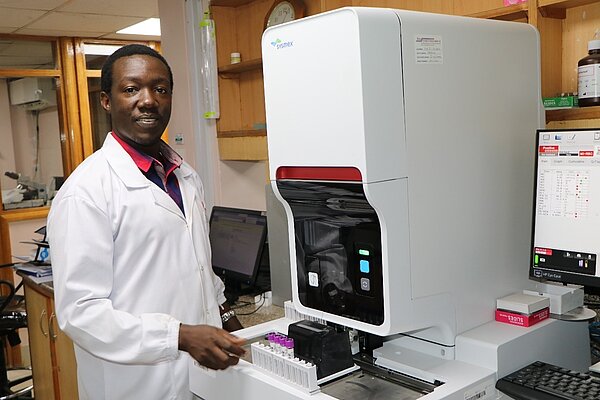
Interview with Dr Simon Onsongo: one step closer to eliminating malaria with automated testing
Interviewer: Victorine Ngetich, Sysmex East Africa
About Dr Simon Onsongo: Dr Onsongo is medical doctor working as a consultant pathologist and the Head of Pathology at the Aga Khan Hospital, Kisumu in Kenya. Aga Khan Kisumu is part of the Aga Khan Health Services, which is one of three leading agencies of the Aga Khan Development Network (AKDN). He completed his undergraduate degree (MBChB) from University of Nairobi, Masters in Clinical Pathology from Aga Khan University (AKU) and MSc in International Healthcare management from University of Essex. He has authored several peer-reviewed publications and served in various advisory roles in hospital, national and international committees. He is passionate about leadership, quality, and clinical research in laboratory medicine in Kenya and beyond.

Dr Onsongo, can you give us a brief description of your day-to-day situation like in your lab?
The Aga Khan Hospital, Kisumu Laboratory, is part of the Aga Khan Health Services. Aga Khan Health Services provides health services in their over 200 multi-level facilities in East Africa, Central/South Asia, and Middle East. In Kenya, Aga Khan Hospital, Kisumu serves people in the western Kenya region, supported by 13 outreach medical centres spread across the western Kenya region arranged in a hub-and-spoke model. Our laboratory provides services to both inpatient and outpatients. Our main hospital offers both inpatient and outpatient services. We also offer both basic laboratory, routine tests for our patients as well as advanced diagnostic support covering both infectious conditions and non-infectious conditions. We offer diagnostic malaria testing using microscopy services (QBC technique) and antigen testing, depending on what our client needs. On average we get between 50-100 requests for malaria tests each day in our main laboratory.
Are there any specific pain points that you think need to be addressed when it comes to malaria testing in your institution?
Globally malaria is still considered a major disease killing many, many people. In 2021, WHO estimated that there were over 200 million cases resulting in over 600,000 deaths, making it a major killer disease. On a global scale, Africa has the biggest disease burden with over 95% of malaria cases and over 96% of deaths occurring in the African continent, so it's really a big problem for us here. Malaria mostly affects children under 5 and pregnant women.
So really, malaria is an endemic disease condition in our setting with ongoing all-year transmission. Although, we have seen a decrease in number of cases over the last years because of the various public health interventions around it. For the longest time microscopy has been the mainstay of malaria diagnosis and I know that proficiency in malaria microscopy can be a challenge for many. You need people who are well-trained, expert microscopists. You need well-stained slides to be able to visualise the parasites. You need electricity and other supplies making reliable and accurate microscopy a labour-intensive process and that's why some people really prefer the use of antigen tests, which are much easier to use in in their facilities.
Since you mentioned malaria testing at your institution, what's roughly the turnaround time for malaria tests in your laboratory?
Our turnaround time for malaria tests is one hour and the service is available 24/7. We mostly use QBC technique in most cases and then electronically transmit the results to our doctors. And for those who are coming from outside, we issue them with printed reports. Rapid antigen testing is also available with a one hour turnaround time.
What do you think prompted you to get or acquire the XN-31 for evaluation and maybe eventually adopting it in your laboratory?
We are evaluating this instrument now. My interest in the instrument was elicited by the study from South Africa by Pillay et.al, which showed that the XN-31 is 100% sensitive, 100% specific, so I was keen to follow up and find out more about this instrument that can be able to solve our malaria diagnostic malaria challenges. This is really a major leap, looking back at standard diagnosis, which started 100 years ago with just the microscopy, and that remains the gold standard. So, hearing of the XN-31 as an automated malaria diagnostic method really excited me and that's why I got in touch with the local Sysmex vendor to see if we could really evaluate and see if this 100% sensitivity and specificity is correct. So far, we're in the middle of the evaluation. I don't have any results in terms of performance now, but soon enough we will be able to share results, and I have no doubt the results will be exciting.
Why do you think analyser such as the XN-31 is vital in the fight against malaria?
Prior to 2010, the majority of our clinicians used presumptive malaria treatment approach where a patient comes with symptoms, the doctor will examine the patient and if they have fever and other suggestive malaria symptoms, they will start treatment. In 2010 the WHO prioritised ‘test and treat’ for malaria diagnosis. This requires someone to do a malaria test, confirm presence of parasites – that’s a parasitological diagnosis – and then offer the treatment. So that really pushed the effort to the laboratories to be able to support patients with parasitological diagnosis.
Early diagnosis and treatment of malaria is important to avoid complications resulting from malaria. At the moment, most people rely on microscopy as the gold standard and know that microscopy has its own challenges. You need well-trained competent people, well-stained slides, and functional microscopes. Adoption of rapid antigen tests has been on the increase. Although antigen tests are easy to use, they have their own challenges. They have lower sensitivity, especially with low parasitaemia patients. The antigen tests only offer qualitative results, and in some cases, it remains positive for a prolonged period of time, up to one month post treatment in some cases. This reduces their utility in follow up.
The XN-31 is elevating the malaria diagnostic game to another level that we haven’t seen before and it's really something that the world has been looking forward to having in terms of the fight against malaria.
And that's why having a machine like XN-31 really adds a lot of benefits. Automation frees up technologists’ time and reduces the turnaround time for running malaria tests. The XN-31 takes about a minute per test to provide results. It provides quantitative results, in terms of the number of parasite-infected red cells and can help speciate in some cases, especially those with P. falciparum. This means that the XN-31 is elevating the malaria diagnostic game to another level that we haven’t seen before and it's really something that the world has been looking forward to having in terms of the fight against malaria.
And really, diagnosis is a core pillar in the global fight against malaria. By treating, you also prevent the transmission. So XN-31 really ticks many of the boxes for an ideal diagnostic test for malaria because of the various things I mentioned above.
Also something that is really good is the additional information you get from XN-31 reports. You get the CBC reports, which will be able to help the clinician to make decisions. For example, if they have a patient with low platelets, they can take note and manage. If the patient has a low HB (haemoglobin), then there may be a need for a transfusion. So that additional information in one run, in one test makes it really an ideal test for us. So, I hope that the evaluation will be successful and we’re able to roll this out on a wider scale around the world.
Is the limit of detection of the XN-31 also something that brings value to your lab and to your patients?
Yes, the limit of detection is important. For example, if you look at the performance of antigen tests, the detection limit is not good at low parasitaemia levels. So, any patient with malaria with parasitaemia below 200 parasites per microlitre, the sensitivity is poor. Microscopy can detect lower parasite counts better than antigen kits but must be done by very competent microscopists. In this regard, the reported limit XN-31 of 20 parasites per microlitre sounds very promising. Such lower detection levels almost rivals PCR as a method, which is still the gold standard in terms of sensitivity.
What impacts do you think COVID-19 pandemic has had on the fight against malaria?
COVID-19 has changed our lives in so many ways. I think the last two years have been tough with public health systems taking a hit. Access to healthcare was really impacted by COVID-19. Many public health interventions such as malaria chemoprevention, distribution of long-lasting insecticide-treated mosquito nets, vaccination and patient visits to hospitals were affected. So, in that way, COVID-19 really limited operations in the public health space.
There's also a bit of the other side where there was a shift of focus away from malaria as a disease to COVID-19. So even companies that were manufacturing malaria rapid diagnostic tests shifted to COVID-19 production to support the pandemic response. In terms of resources, the healthcare system really focused on COVID-19 and rightly so. The WHO estimates during 2021, there were almost 47,000 deaths due to that shift alone. I think now that COVID-19 is going down, we hope that the efforts can go back again to malaria, and we will be able to implement the various public health interventions that were there, not only for malaria, but also other important public health priorities.
Antimicrobial resistance covers resistance to antimalarial medication. From your perspective, do you think using the XN-31 will have an impact on reduction of AMR against antimalarials?
I think it will. With a quick diagnosis, you can start targeted treatment quickly – and that means that you break the transmission cycle for malaria. The use of antimalarials will be more targeted so that people who are not sick are not given antimalarials and they are only used when indicated because resistance is really a problem around the world. Proper and effective use of antimalarials is important to be able to preserve their longevity and having a method of diagnosis that is accurate, sensitive and specific really boosts the fight against AMR for antimalarials.

How does malaria testing with the XN-31 analyser align with your organisational goals and objectives?
Aga Khan Kisumu is on the path to becoming a centre of excellence for infectious disease in the region. Our dream is to be the go-to centre of excellence when it comes to various kinds of infectious diseases. We've started to make strategic investments and partnering with the right partners as we journey towards our goal.
Getting to work with Sysmex and being able to work with the XN-31 is really part of our agenda to be able to excel in diagnostics and that really adds on to our services and core values of providing the best services in infectious diseases. We are really very proud of our partnership with Sysmex and being the first institution in Kenya to be able to have our hands on the XN-31, and so far, it's looking promising, and I look forward to better and the greater partnerships regarding malaria and beyond.
Is there anything else you would like to add?
I have one quote which I wanted to share from our WHO director Tedros Adhanom Ghebreyesus. “Malaria has afflicted humanity for millennia. We have the tools and the strategy now to save many lives – and with new tools, to start to dream of a malaria-free world.” I found it interesting because malaria has been with us for many, many centuries and to have these tools now, it will hopefully provide us with that future without malaria.



