Fighting multidrug resistant bacteria in urology – awareness and education is key
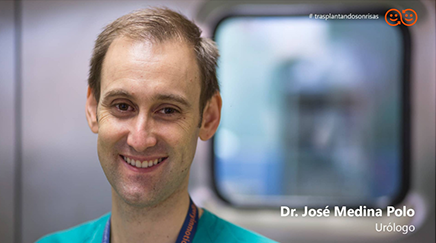
Dr José Medina-Polo, PhD in Medicine-Surgery, is a member of the urology faculty in the Department of Urology at the Hospital Universitario 12 de Octubre, HM Hospitales & ROC Clinic in Madrid, Spain. Since 2016 at this hospital, he has also been a member of the Commission on Healthcare Associated Infections, Prophylaxis and Antibiotics. He’s also a member of the Commission on Healthcare Associated Infections (HAI) at his hospital, which decides on local strategies and awareness actions.
We conducted an interview with Dr José Medina-Polo, where he discusses his experience in the field of urology with urinary tract infections, multidrug resistant bacteria (MRB) and antimicrobial resistance (AMR). Keep reading to find out what he thinks will help slow down the development of resistance and what urologists can do specifically to play their part in the fight against MRB and AMR.

For us urologists, it is very important to get analysis results, e.g. urine or blood cultures, as fast as possible.
Does AMR have a measurable economic impact on the treatment of patients in the urology field? Is there a measurable impact on the resources that we need to treat urinary tract infection (UTI) patients due to antimicrobial resistance (AMR)?
I don’t have the numbers on that, but it is true that hospital acquired infections (HAI) patients affected by multidrug resistant bacteria (MRB) have a higher hospitalisation rate and the hospitalisation period is clearly longer. If we consider that, according to calculations in the United States, a UTI patient bed costs around $900/day, the influence is clear. On top, the antibiotics that we use to treat such kind of infections are more expensive than first line antibiotics and the duration of the treatment is longer. Furthermore, the demands on the healthcare system in terms of resources increase, since such patients are referred to the urologist and the case requires an evaluation by a PROA (Programme for the Optimisation of the use of Antibiotics) committee, which increases the indirect costs. After an infection with a MRB, it is also required to have a urine culture after the infection to ensure successful treatment. With those points, we are naturally not considering the costs associated to patient morbidity.
Do you see patients who suffer from infections caused by multidrug resistant bacteria in the everyday practice, or are we still talking about isolated cases?
The rate of infection with MRB among UTI patients who require hospitalisation in our hospital is 20%, which points out to HAI. Concerning community-acquired infections, the statistics in the region of Madrid show around 3-4% of the cases being MRB infections. This is a relevant figure, considering that we observed less than 1% only 20 years ago.
The number of MRB infections has clearly escalated during the last year, due to the increased prescription of antibiotics derived from the COVID-19 pandemic. This observation is not only applicable to the urology department, but to the whole hospital. MRB has not only affected COVID patients; the trend has also been observed in patients who had to be admitted to the hospital because of other reasons.
In my mind, the way forward is very clear and can be described with a single word: education.
How often do UTI patients end up developing urosepsis or even sepsis? Is this kind of complication a reality in the urology practice?
It really depends on the patient’s profile and medical history. If we take pre-menopausal women without any comorbidities as reference, it is not usual that a UTI evolves to generate sepsis. The picture changes if we consider rather complicated UTIs. In patients with malformations in the urinary tract or who are affected by urinary lithiasis, sepsis is a reality. We do observe many lithiasis patients who develop sepsis starting from a UTI.
Luckily, MRB are not so common in community-acquired infections. In patients who are in contact with the healthcare system though (have received lithiasis treatment, catheter patients, transplant patients, etc.), infections with MRB are a real risk. That’s why it’s so important to classify patients according to the complicated/uncomplicated criteria.
And that highlights the relevance of the determination of the bacteria affecting UTI patients and their Antibiotics susceptibility/resistance pattern.
Indeed. The most important point is performing observational studies. Only then can you determine the real situation of the patient based on risk factors. As a result of internal observational studies, we could determine some key risk factors of suffering a MRB infection, such as insertion of catheters in the upper urinary tract or certain types of surgery. We treat those patients as MRB infection ones to prevent complications. Thus, it’s key to analyse your own data to establish the factors to define the risk profile, otherwise, you’re blindfolded when deciding on which treatment to prescribe. Observational studies are important to adapt your treatment decisions to the reality observed in your local community. This should be supported by scientific societies and the administration.
When we talk about gathering as much information about the patients as possible, we come close to the diagnostics topic. From your point of view, what diagnostic tools are missing in urology?
Where should the diagnostics industry set its focus in new developments?
In addition to observational studies, the time-to-results is a major factor. For us urologists, it is very important to get analysis results, e.g. urine or blood cultures, as fast as possible. As long as we don’t have those results, and currently that waiting time can be two days, we are blindfolded when deciding on therapeutic options. We need to know the risk factors of the patient, have access to rapid results and then adapt the antibiotics required in that particular case, to use the most indicated drug. This way we can minimise the development of antibiotic resistance in the long run.
In terms of moving forward we really need to coordinate our efforts. What is being done at this moment at your local level (in your hospital, in the region of Madrid…) to coordinate the fight against AMR?
In my mind, the way forward is very clear and can be described with a single word: education. Of course, how to build that path is a complex issue, since we need to include all the links in the chain: doctors, nurses, patients, but also family and other hospital staff. In our case, in the urology service in the hospital, we started 10 years ago with the analysis of our situation (observational study), creation of specific protocols and training of the hospital staff (at all levels, warden, doctors, nurses, etc.). We created a set of recommendations for patients and their families. The hospital also contributed by facilitating material to prioritise hygiene. We also implemented a tutoring/coaching programme, in which a practitioner specialised in infectious diseases observes procedures done by colleagues and coaches if the required measures are not followed.
As it happens with many other topics, the world needs a coordinated, unified answer to AMR. It won’t be efficient if only local initiatives with individualised protocols are implemented.
We are also active in social media. Our hospital has posted videos targeting the general public to explain how pathogens are transported and transmitted, etc. I just saw a TV campaign the other day from our Ministry of Health about avoiding the use of antibiotics to treat a cold or a flu. While these campaigns might not make all the public change their mind, we might reach some people, who then stick to good practices.
Interestingly, while the COVID-19 pandemic is having a negative influence on AMR, it also has a positive influence on prevention. Everyone is now more familiar with hygiene measures and tries to break transmission chains. That’s an example how education, in a broad range, can work.
Concerning awareness campaigns, do you think that the administration is actively involved in that? Does the problem receive attention and resources from the administration?
Yes, it is a priority for the administration and resources are being allocated to create awareness. The problem is, however, that the actions undertaken are not properly reaching healthcare professionals and the general public. Following what’s being done in other countries, we need to work on how we make the message reach the public. State and regional authorities are running studies regularly to assess the development of AMR and launch awareness campaigns. The impact they have outside the medical community is, though, limited.
Talking about the patients… Do the patients you see in the daily practice understand AMR? Are they aware about the problem and the limitations of antibiotics?
That is clearly improving. Only five years ago, many patients expected antibiotics prescription for UTIs. The current case for urologists, who treat very often recurrent UTIs, is the opposite. Many patients who have been previously treated with ABx ask their doctor to avoid, if possible, new antibiotics prescription. Somehow, they have realised that antibiotics is not necessarily the solution. This attitude change has become clearer within the last few years. We see that this concern is shared, at least, by those patients who have already received antibiotics treatment.
While not trying to philosophise about the topic, one could ask himself the question of where we are headed in terms of AMR? Should we be concerned, or even afraid, or do we still have chances to change the development?
Short answer: both are correct. It is certain that AMR is going to cause deaths and increased morbidity in the future. At the same time, medicine keeps evolving and it will offer us tools to hinder the development of AMR. We need to understand that AMR will continue growing. We also need to consider that, within the last decades, practically no new antibiotics have been developed. All in all, it is a problem, and we will see deaths caused by MRB, but we are, step by step, implementing tools to deal with it. While we are already putting measures in place, the pace of change needs to be increased.
Still, I see light at the end of the tunnel. I think we should be optimistic since we have regular campaigns and they are contributing to the fight. The change in our patients’ perception of antibiotics is already tangible – more and more patients are concerned about the dangers of the use of antibiotics.
One of our main concerns should be AMR development in countries with limited resources and where the healthcare system is not very well developed. In these cases, moving forward and creating and implementing protocols to fight AMR will certainly be more challenging. As it happens with many other topics, the world needs a coordinated, unified answer to AMR. It won’t be efficient if only local initiatives with individualised protocols are implemented.
Having homogeneous protocols really looks like the way to go. As we have recently seen with the pandemic, it is not effective if efforts are not coordinated at international level. Are we already at that stage, at least, in Europe?
I think so. Particularly in the urology field, the European Association of Urology has done important work in gathering data from across Europe. Even if bacterial strains and their resistance patterns are not fully comparable between different European countries, the EAU has unified the protocols and decision criteria on how to proceed in each case, including diagnostic steps. We now have homogeneous protocols and recommendations of treatment.
Nevertheless, these homogeneous protocols must be put in the local context. In my opinion, the future includes using new technologies to input the characteristics of the patient to get a personalised diagnostic answer, adapted to that person and the bug affecting them. The output we need to achieve is creating tools that yield the answer: the antibiotic indicated to treat this patient is X. This also includes selecting antibiotics within the results of an antibiogram to extend the life of existing antimicrobials.
Any further comments?
Our homework as urologists is to pay attention to asymptomatic bacteriuria. Asymptomatic patients have historically been treated, although it has been demonstrated that such treatment is contraindicated. In the end, the treatment of asymptomatic patients is associated to more symptomatic infections afterwards and to increased AMR. We are aware that asymptomatic patients systematically receive treatment – that should be avoided, as all guidelines advise not to treat those patients with antimicrobials.


